Vaccination is a critical component of disease prevention in public health. Among the various types of vaccines available, inactivated or killed vaccines hold a significant place. Unlike their live attenuated counterparts, these vaccines are made from pathogens that have been killed or inactivated with chemicals, heat, or radiation. This crucial feature ensures that these pathogens cannot revert to their disease-causing form.
The Development Process of Inactivated Vaccines
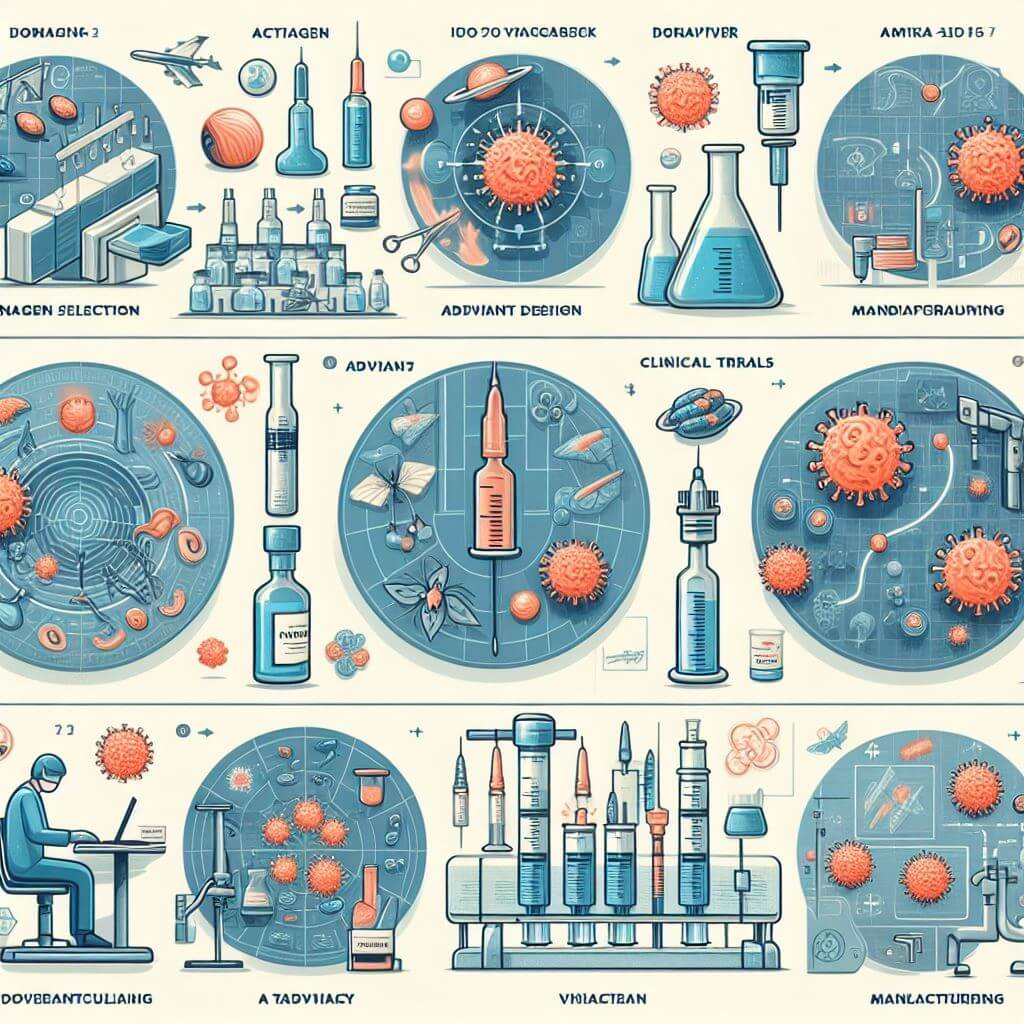
The process of developing inactivated or killed vaccines is intricate and requires precise scientific techniques to ensure the resulting product is both safe and effective for public use. The initial step is the selection and cultivation of the virus or bacterium that will be the basis for the vaccine. This pathogen must be grown under controlled conditions, often in large quantities, so that there is enough material to work with. Scientists typically use specific cell cultures, eggs, or other growth media designed to support the growth of the pathogen without allowing it to cause disease.
Once enough pathogens are grown, they are then subjected to an inactivation process. The goal is to destroy the pathogen’s ability to replicate and cause illness without affecting the structure of its antigens—the critical pieces that trigger the immune response. The methods of inactivation vary but include the use of chemicals like formaldehyde or beta-propiolactone, application of heat, or exposure to radiation. Selecting the appropriate method is vital since it must effectively neutralize the pathogen while preserving its antigenic properties.
 After the pathogen has been effectively inactivated, a series of purification steps follow. These ensure that any materials used during the cultivation and inactivation phases, along with other extraneous proteins or components that could act as contaminants, are removed. Purification is crucial because it reduces the risk of potential side effects and increases the vaccine’s safety profile. Too much purification can sometimes remove parts of the pathogen needed to elicit a robust immune response, while too little can result in an impure vaccine.
After the pathogen has been effectively inactivated, a series of purification steps follow. These ensure that any materials used during the cultivation and inactivation phases, along with other extraneous proteins or components that could act as contaminants, are removed. Purification is crucial because it reduces the risk of potential side effects and increases the vaccine’s safety profile. Too much purification can sometimes remove parts of the pathogen needed to elicit a robust immune response, while too little can result in an impure vaccine.
Once the vaccine antigen is purified, it may then be mixed with adjuvants, substances that enhance the vaccine recipient’s immune response. Adjuvants can increase the efficacy of the vaccine by helping to present the antigen to the immune system in a more effective way. Alum, or aluminum salts, is a common adjuvant used in many inactivated vaccines.
In addition to adjuvants, stabilizers are added to preserve the vaccine’s effectiveness during storage and transport. These substances are crucial for ensuring that the vaccine can be delivered to diverse climates and settings without losing its potency.
Each batch, or lot, of vaccine goes through a rigorous process of quality control testing, including tests for sterility, potency, and purity. These tests are designed to ensure that each dose of vaccine is consistent with the last and that they all conform to the standards set by regulatory bodies such as the Food and Drug Administration (FDA) in the United States or the European Medicines Agency (EMA) in Europe. These regulatory agencies require extensive documentation and evidence of safety and efficacy before a vaccine can be approved for public use.
Once a vaccine has passed all necessary testing and has been approved, it enters production, where it will be manufactured at a larger scale. Even during production, samples from each lot are continually tested to ensure high quality is maintained. After manufacturing, the vaccine is distributed to healthcare providers around the world, becoming a key defense in the fight against infectious diseases.
The Mechanism of Immunity with Inactivated Vaccines
The underlying principle of any vaccine is to prime the immune system to defend against a specific pathogenic threat without exposing it to the risk of a full-blown infection. Inactivated vaccines accomplish this by introducing antigens from killed pathogens into the body. Antigens are molecular structures on the surface of pathogens that the immune system can recognize as foreign. The uniqueness of inactivated vaccines lies in their inability to replicate, thereby eliminating the risk of causing the diseases they are designed to prevent.
When an inactivated vaccine enters the body, the immune response is initiated by antigen-presenting cells, such as dendritic cells, which digest the inactivated pathogen and present its antigens on their surface. This action captures the attention of two critical players in the adaptive immune system: T-lymphocytes and B-lymphocytes, often referred to as T-cells and B-cells, respectively.
T-cells come in various types with different roles. Helper T-cells, specifically, play a pivotal role in orchestrating the immune response by releasing cytokines, which signal B-cells and other immune cells to react. On the other hand, cytotoxic T-cells are critical for killing infected cells directly, although their role is less prominent in response to inactivated vaccines due to the absence of live pathogens to infect host cells.
B-cells are the producers of antibodies in the immune system. Once they are activated by the help of T-cells and the presence of the antigen, they differentiate into plasma cells, which are essentially antibody factories. These antibodies are tailored to the specific antigens present on the vaccinated pathogen. They circulate throughout the bloodstream, ready to interact with the pathogen if it should ever invade the body. By binding to the pathogen, antibodies can neutralize it, preventing it from entering cells, or mark it for destruction by other immune cells.
Another significant outcome of the immune response to inactivated vaccines is the creation of memory cells. B and T memory cells are specialized cells that remain in the body long after the initial exposure to the vaccine. These cells have a longer lifespan and stand at the ready to quickly expand and mount a powerful response upon subsequent exposure to the pathogen. Memory cells are the reason why, after vaccination, the body can respond to an infection more rapidly and forcefully, often preventing the disease from developing.
Despite the effectiveness of inactivated vaccines, the immune response they elicit can sometimes be less powerful or shorter-lived than the response induced by live attenuated vaccines. This is primarily because inactivated pathogens do not replicate inside the body, resulting in a less robust stimulation of the immune system. To counter this, inactivated vaccines are frequently administered in multiple doses. The initial dose, or primary vaccination, primes the immune system, while subsequent booster shots serve to re-expose the immune system to the antigen, thereby enhancing and prolonging the immune response.
The inclusion of adjuvants in many inactivated vaccines amplifies the immune response without the need for the pathogen to replicate. Adjuvants work by boosting the body’s immune response to the vaccine, making it more effective and sometimes allowing for smaller quantities of the vaccine antigen to be used.
Efficacy and Safety of Killed Vaccines
One of the benefits of inactivated vaccines is their safety. Because the pathogens can no longer replicate, there is no risk of the vaccine causing the disease it aims to protect against. This trait makes inactivated vaccines particularly suitable for individuals with weakened immune systems, who may be at higher risk of complications from live vaccines.
As the immune response to inactivated vaccines is typically weaker than that to live vaccines, boosters are often necessary to maintain immunity. Depending on the vaccine, it may be necessary to administer additional doses every few years to ensure ongoing protection.
The safety profile of inactivated vaccines is generally favorable. The lack of live components minimizes the risk of vaccine-induced disease. Most side effects are mild and temporary, such as soreness at the injection site, low-grade fever, or fatigue. Serious adverse reactions are extremely rare and are vigilantly monitored by health agencies.
In terms of efficacy, inactivated vaccines have successfully controlled and, in some cases, eradicated diseases. Polio, for example, has been nearly eradicated thanks to a widespread vaccination campaign using the inactivated poliovirus vaccine (IPV). The hepatitis A vaccine is another inactivated vaccine that has markedly reduced the incidence of the disease in populations with routine vaccination programs.