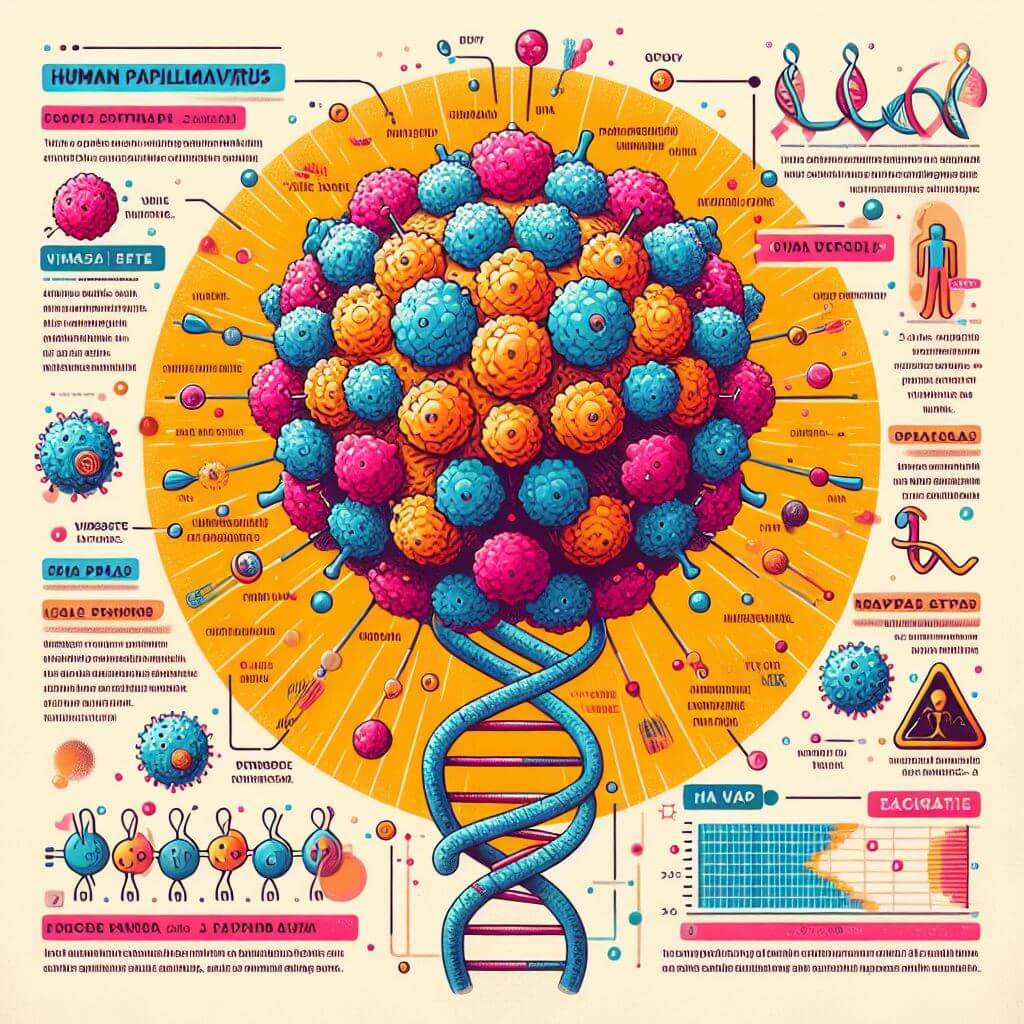
Human papillomavirus, more commonly known as HPV, is a term that refers to a group of viruses. With more than 100 different types, HPV is ubiquitous in human populations, making it the most common sexually transmitted infection (STI) worldwide. HPV is spread mainly through intimate skin-to-skin contact, not just during sexual intercourse. This means that it can be transmitted through any sexual contact, which makes its distribution widespread.
Understanding the health consequences of human papillomavirus (HPV) is vital for both individuals and healthcare professionals. While it is true that most HPV infections do not lead to serious health problems and often resolve spontaneously, the real concern is the virus’s potential to cause long-term health problems. Among the wide variety of more than 100 types of HPV, some strains are particularly dangerous and can lead to various forms of cancer and warts.
 Genital warts are one of the most visible signs of HPV infection. They can appear as small bumps, groups of bumps, or stalk-like bumps in the genital area, and in some cases, they can become quite large and cause discomfort or even pain. Although they are usually associated with strains of HPV that are considered insignificant for the development of cancer, their presence is a clear indication of HPV infection and can cause distress or embarrassment to patients.
Genital warts are one of the most visible signs of HPV infection. They can appear as small bumps, groups of bumps, or stalk-like bumps in the genital area, and in some cases, they can become quite large and cause discomfort or even pain. Although they are usually associated with strains of HPV that are considered insignificant for the development of cancer, their presence is a clear indication of HPV infection and can cause distress or embarrassment to patients.
The more sinister aspect of HPV lies not in these visible manifestations, but in its silent ability to cause cancer. High-risk HPV strains, particularly HPV 16 and 18, are directly associated with several types of cancer. Cervical cancer is the most common malignancy, with HPV accounting for nearly 99% of cervical cancers worldwide. However, its influence does not end there. HPV is involved in a significant percentage of anal, oropharyngeal, vulvar, vaginal, and penile cancers. The virus can remain unnoticed in the body for years, causing changes in cellular structures that can eventually develop into cancer.
For women, regular screening with Pap smears (or Pap tests) and HPV DNA testing is an important line of defense. These tests can detect precancerous changes in the cervix that can turn into cancer if left untreated. Understanding the relationship between HPV and these serious health outcomes highlights the importance of early detection and prevention strategies.
For both men and women, the potential for HPV to lead to oropharyngeal cancer is a growing concern. The incidence of these cancers has been increasing in recent decades, especially among men. The association between HPV and oropharyngeal cancer underscores the need for awareness and research into prevention and treatment options for all genders.
Although cervical cancer screening methods are available, screening for other HPV-related cancers is not as straightforward, making prevention through vaccination and safe practices even more important. The health consequences of HPV are far-reaching, affecting not only individual well-being but also public health. Understanding these effects is the first step in combating the widespread impact of this virus.
Prevention and Vaccination
Prevention and vaccination are key to the global fight against human papillomavirus (HPV) and its subsequent health consequences. Because HPV is the most common sexually transmitted infection with widespread prevalence and potentially severe consequences, the development of preventive vaccines represents a major public health advance. The HPV vaccine effectively provides immunity against the most harmful strains of the virus, protecting against most types of cervical cancer, as well as various other types of cancer and genital warts associated with HPV.
The importance of vaccination cannot be overemphasized. The vaccine is most effective when given before people become sexually active, so it is recommended for teenage boys and girls. This time ensures the development of immunity to any contact with HPV. However, vaccination is not limited to this age group; it can be administered to persons from 9 years to 45 years of age. Those who missed vaccination at the recommended age are recommended to get vaccinated. This wide recommended age range for vaccination reflects the universal risk associated with HPV and the benefits of protection at any stage of sexual life.
Vaccination campaigns face the challenge of misinformation and vaccine hesitancy caused by misconceptions about vaccine safety and the stigma associated with sexually transmitted infections. Education and clear communication are critical to overcoming these barriers. Health professionals play an important role in discussing HPV and vaccines with both parents and youth, dispelling myths, and emphasizing vaccine safety and effectiveness in preventing certain cancers and diseases.
Prevention goes beyond vaccination. Safe sex practices, including the use of condoms, can reduce the risk of HPV transmission. However, it is important to note that although condoms can reduce the risk of HPV infection, they do not provide complete protection against the virus due to the possibility of contact with infected skin that is not covered by a condom. Therefore, vaccination remains the most effective method of HPV prevention.
Early screening complements vaccination in the prevention strategy of HPV-related diseases. For women, regular cervical cancer screenings, such as Pap and HPV DNA tests, are important for early detection of precancerous changes. There is no standard HPV screening test for men, but high-risk individuals, such as men who have sex with men or HIV-positive individuals, may need anal cancer screening.
HPV – Society’s Responsibility
The fight against human papillomavirus (HPV) goes far beyond individual actions; it requires the collective commitment of communities around the world. The prevalence of HPV, combined with its potential to cause serious health problems, underscores the need for a unified approach to prevention, education, and support. Community responsibility in the context of HPV involves comprehensive health initiatives, education programs, and open conversations aimed at reducing the transmission and impact of the virus.
Education is the cornerstone of community efforts. Although HPV is the most common sexually transmitted infection, there are widespread misconceptions and a lack of knowledge about its transmission, consequences, and methods of prevention. Communities can play a significant role by implementing educational programs targeting different age groups, including teenagers, parents, and the elderly. These programs should include information about how HPV is transmitted, the potential health risks associated with the virus, and the primary importance of vaccination and regular health checkups. By integrating HPV education into school curricula and community health initiatives, we can create an environment where informed decisions about health and sexuality are the norm.
Public health efforts should also focus on increasing the availability and acceptability of the HPV vaccine. This involves not only providing the vaccine to all eligible individuals but also working to normalize its administration as part of routine medical care. Communities can achieve this by organizing vaccination campaigns, offering vaccines at a reduced cost or free to low-income populations, and by having healthcare providers actively recommend the vaccine during medical consultations. Moreover, public health campaigns can directly confront vaccine skepticism by debunking myths and presenting facts about vaccine safety and efficacy through trusted community leaders and health professionals.
Equally important is the creation of a culture of openness and support. The stigma associated with sexually transmitted infections, including HPV, often leads to silence, fear, and avoidance of needed health care or vaccination. Community leaders, educators, and health professionals can encourage open dialogue about sexual health, eliminating the stigma and embarrassment that can be associated with these topics. Support groups, community forums, and even social media platforms can offer places to share experiences, provide support, and share accurate information.
In addition, advocating for policy changes that support HPV prevention efforts, such as making the vaccine more accessible and affordable, and providing comprehensive sexuality education in schools, are key steps that can be taken at the community level. Through petitions, public forums, and engagement with politicians, communities can influence the wider society and political environment in favor of proactive HPV prevention and treatment strategies.