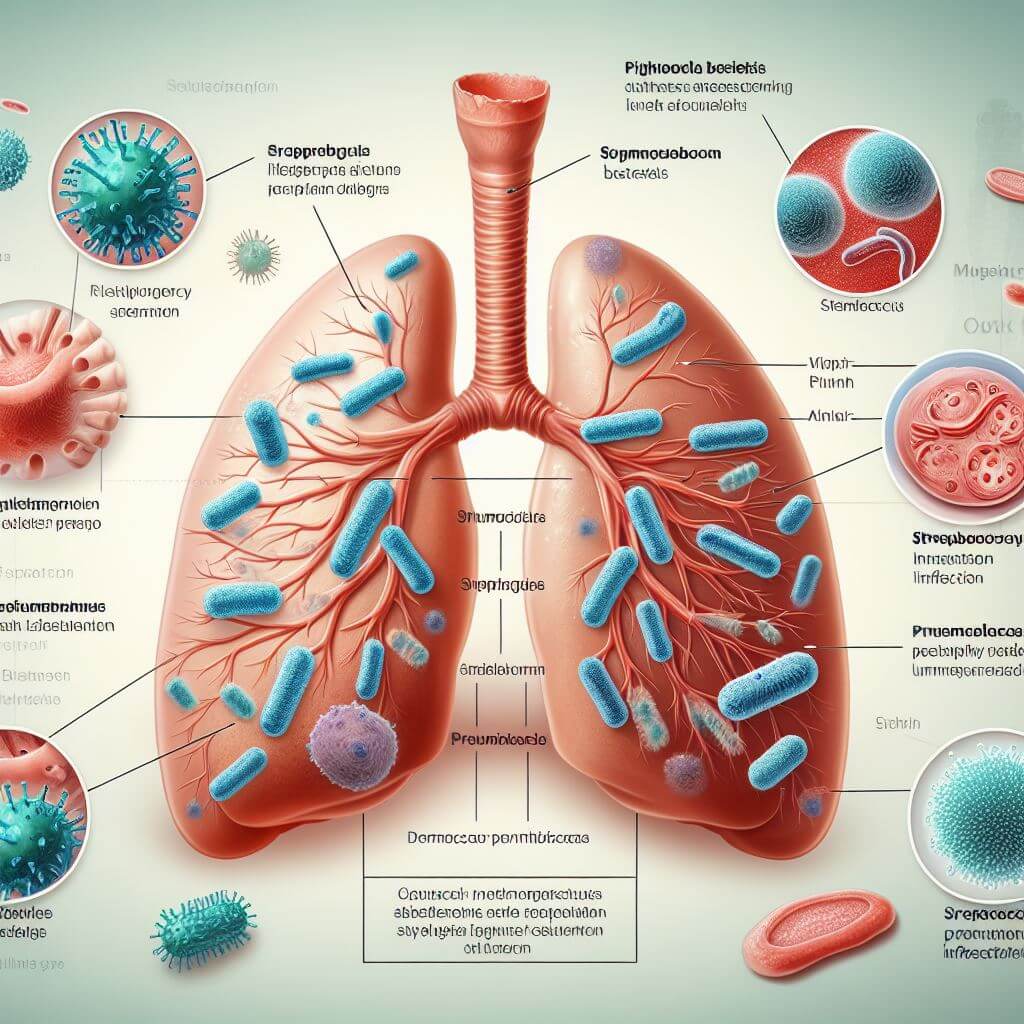
Understanding pneumococcal infection is fundamental to recognizing the importance of preventive measures such as vaccination. This disease is caused by the bacteria Streptococcus pneumoniae, commonly known as pneumococcus, which is infamous for its ability to cause several severe infections. These infections can take many forms, including pneumonia, which affects the lungs; meningitis, an infection of the protective membranes of the brain and spinal cord; and bacteremia or sepsis, which are bloodstream infections. These conditions are not only potentially life-threatening, but also create a significant health burden, leading to hospitalization and, in severe cases, long-term complications or death.
Pneumococcus is particularly dangerous because it is easily spread by coughing, sneezing, or close contact with an infected person. This makes everyone potentially at risk, although some groups are more vulnerable than others. Young children, the elderly, and people with weakened immune systems or certain chronic illnesses face a higher risk of pneumococcal infection. This increased vulnerability is partly due to their less robust immune defenses being able to fight off the bacteria.
The ability of Streptococcus pneumoniae to develop resistance to antibiotics has complicated the treatment of pneumococcal infection. Over the years, the misuse and overuse of antibiotics have accelerated the emergence of drug-resistant strains of bacteria, making some infections more difficult to treat. This resistance highlights the need for effective preventive measures, such as vaccination, to manage and control the impact of pneumococcal infection.
 Given its widespread impact and the challenges of antibiotic resistance, understanding pneumococcal infection is not just about recognizing its symptoms and treatment options. It is also about recognizing the critical role of prevention, particularly through vaccination, in protecting vulnerable populations and reducing the incidence and severity of this potentially devastating condition. Thus, public awareness efforts about pneumococcal disease and the importance of vaccination are key components of public health strategies aimed at combating this threat.
Given its widespread impact and the challenges of antibiotic resistance, understanding pneumococcal infection is not just about recognizing its symptoms and treatment options. It is also about recognizing the critical role of prevention, particularly through vaccination, in protecting vulnerable populations and reducing the incidence and severity of this potentially devastating condition. Thus, public awareness efforts about pneumococcal disease and the importance of vaccination are key components of public health strategies aimed at combating this threat.
The Role of Vaccination
The role of vaccination in the fight against pneumococcal infection is difficult to overestimate. Vaccines serve as an important line of defense, forcing the immune system to recognize the bacterium Streptococcus pneumoniae and effectively fight it in the event of infection. This preventive approach has proven to be one of the most effective means of reducing the incidence of pneumococcal disease, which can range from mild to life-threatening depending on the person and the type of infection.
Pneumococcal vaccines are divided into two main types: pneumococcal conjugate vaccines (PCVs) and pneumococcal polysaccharide vaccines (PPSVs). Each plays a unique role in the immune defense designed to provide the most effective coverage against many strains of bacteria. PCV targets the most common and aggressive strains of pneumococcus, making it particularly suitable for infants and young children, who are among the groups most at risk of severe disease. This vaccine works by conjugating, or binding, a part of the bacteria’s envelope to a protein that helps the body’s immune system recognize and remember the bacteria, thus providing better and longer-lasting protection.
In contrast, PPSV targets a broader range of pneumococcal strains and is recommended for adults 65 years of age and older and people 2 to 64 years of age with certain risk factors or medical conditions. It stimulates the immune system to produce antibodies against many types of pneumococcal bacteria, protecting a wider range of pneumococcal diseases. However, it may not elicit a strong immune response in all recipients, so the conjugate vaccine is best given to children under 2 years of age.
Widespread implementation of pneumococcal vaccination programs has led to a significant reduction in the incidence of pneumococcal diseases among the vaccinated population. These vaccines not only protect the people who receive them, but also contribute to the formation of herd immunity. Herd immunity occurs when a large enough portion of society is immunized against an infectious disease, thereby limiting its spread and protecting those who are not immune. This is especially important for individuals who are medically unable to receive the vaccine, as it reduces their risk of contracting the disease.
However, the role of vaccination goes beyond individual or societal protection. By reducing the number of cases of pneumococcal infection, vaccines also reduce the need for antibiotic treatment, helping to slow the spread of antibiotic resistance. This aspect of vaccination highlights its importance not only in preventing disease, but also in preserving the effectiveness of antibiotics for future generations.
Impact of Vaccination
The impact of pneumococcal vaccination has been profound and multifaceted, reflecting a major public health triumph. The introduction and widespread use of pneumococcal vaccines have resulted in significant reductions in infection rates both among the vaccinated population and the general public, demonstrating the powerful protective effect these vaccines provide against a formidable pathogen.
One of the most striking consequences was a sharp decrease in invasive pneumococcal diseases among children, a group particularly vulnerable to the severe consequences of such infections. Before the widespread use of the pneumococcal conjugate vaccine (PCV), diseases such as pneumococcal meningitis and blood infections were not uncommon and often resulted in serious long-term health problems or, sadly, loss of life. Today, these effects are becoming increasingly rare in countries with high vaccination coverage, indicating the vaccine’s ability to protect children from the most severe effects of pneumococcal infection.
The benefits of pneumococcal vaccination extend beyond the direct protection of individuals receiving the vaccine. Herd immunity, an important public health concept, refers to the indirect protection afforded to unvaccinated individuals when a sufficiently large proportion of the population is immune to an infectious disease. Through this mechanism, pneumococcal vaccination has played an important role in reducing community transmission, thereby reducing morbidity in unvaccinated populations such as newborns or those with certain diseases that prevent vaccination.
Furthermore, the impact of vaccination on health systems and the economy cannot be ignored. By preventing a significant number of cases of pneumococcal infection, vaccines have markedly reduced hospitalizations, medical interventions, and associated healthcare costs. This not only eases the economic burden on families and healthcare systems but also allows for a more efficient allocation of healthcare resources, supporting broader public health and emergency response initiatives.
The widespread use of pneumococcal vaccines has also played a key role in the fight against antibiotic resistance. Reducing the incidence of pneumococcal disease reduces the need for antibiotics, which in turn slows the development and spread of resistant strains of pneumococci. This aspect of vaccination highlights an important, often underappreciated advantage: maintaining the effectiveness of antibiotics for treating a variety of bacterial infections, not just pneumococcal infections.